Abstract
Case Report
Primary central nervous system lymphoma post kidney transplantation: a case report
Souhir Khemiri*, Sonda Masmoudi, Wala Ben Kridis and Afef Khanfir
Published: 03 June, 2022 | Volume 6 - Issue 2 | Pages: 063-067
Introduction: Primary central nervous system (PCNS) posttransplant lymphoproliferative disease (PTLD) is a rare complication of solid organ transplantation and treatment is not yet standardized.
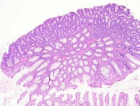
Case presentation: Here we report the case of a 54-year-old man who underwent renal
transplantation 22 years ago for end-stage renal disease. He had been on long-term immunosuppressive treatment consisting of orally administered prednisolone 10 mg and then 5 mg daily and orally administered Mycophenolate Mofetil 500 mg twice daily. He presented in January 2019 to emergency with aphasia and then partial seizure. On brain MRI there was an expansive cortical mass in the left temporal lobe with perilesional edema. Biopsy revealed a diffuse large B-cell lymphoma. He was treated with one cycle of Cytarabine with his usual immunosuppressive treatment. In view of his renal allograft, he was not suitable for Methotrexate due to the risk of toxicity. He died on day 15 caused by a sepsis choc secondary to febrile neutropenia.
Conclusion: PCNS-PTLD is regarded as one of the most serious posttransplant complications due to its high mortality. Further clinical and experimental investigations are required to develop optimal diagnostic and treatment modalities.
Read Full Article HTML DOI: 10.29328/journal.jcn.1001091 Cite this Article Read Full Article PDF
References
- Dharnidharka VR, Webster AC, Martinez OM, Preiksaitis JK, Leblond V, Choquet S. Post-transplant lymphoproliferative disorders. Nat Rev Dis Primers. 2016 Jan 28;2:15088. doi: 10.1038/nrdp.2015.88. PMID: 27189056.
- LaCasce AS. Post-transplant lymphoproliferative disorders. Oncologist. 2006 Jun;11(6):674-80. doi: 10.1634/theoncologist.11-6-674. PMID: 16794246.
- Kim JH, Kim SO, Han DJ, Park SK. Post-transplant malignancy: a burdensome complication in renal allograft recipients in Korea. Clin Transplant. 2014 Apr;28(4):434-42. doi: 10.1111/ctr.12328. PMID: 24750289.
- Quinlan SC, Pfeiffer RM, Morton LM, Engels EA. Risk factors for early-onset and late-onset post-transplant lymphoproliferative disorder in kidney recipients in the United States. Am J Hematol. 2011 Feb;86(2):206-9. doi: 10.1002/ajh.21911. PMID: 21264909; PMCID: PMC3311225.
- Opelz G, Döhler B. Lymphomas after solid organ transplantation: a collaborative transplant study report. Am J Transplant. 2004 Feb;4(2):222-30. doi: 10.1046/j.1600-6143.2003.00325.x. PMID: 14974943.
- Dharnidharka VR.Epidemiology of PTLD. In: Dharnidharka VR, Green M, Webber SA, eds. Post-transplant Lymphoproliferative Disorders. New York City, NY: Springer; 2010: 17-28.
- Evens AM, David KA, Helenowski I, Nelson B, Kaufman D, Kircher SM, Gimelfarb A, Hattersley E, Mauro LA, Jovanovic B, Chadburn A, Stiff P, Winter JN, Mehta J, Van Besien K, Gregory S, Gordon LI, Shammo JM, Smith SE, Smith SM. Multicenter analysis of 80 solid organ transplantation recipients with post-transplantation lymphoproliferative disease: outcomes and prognostic factors in the modern era. J Clin Oncol. 2010 Feb 20;28(6):1038-46. doi: 10.1200/JCO.2009.25.4961. Epub 2010 Jan 19. PMID: 20085936; PMCID: PMC2834429.
- Buell JF, Gross TG, Hanaway MJ, Trofe J, Roy-Chaudhury P, First MR, Woodle ES. Posttransplant lymphoproliferative disorder: significance of central nervous system involvement. Transplant Proc. 2005 Mar;37(2):954-5. doi: 10.1016/j.transproceed.2004.12.130. PMID: 15848587.
- Penn I, Porat G. Central nervous system lymphomas in organ allograft recipients. Transplantation. 1995 Jan 27;59(2):240-4. PMID: 7839447.
- Cavaliere R, Petroni G, Lopes MB, Schiff D; International Primary Central Nervous System Lymphoma Collaborative Group. Primary central nervous system post-transplantation lymphoproliferative disorder: an International Primary Central Nervous System Lymphoma Collaborative Group Report. Cancer. 2010 Feb 15;116(4):863-70. doi: 10.1002/cncr.24834. PMID: 20052713; PMCID: PMC4113953.
- Leblond V, Dhedin N, Mamzer Bruneel MF, Choquet S, Hermine O, Porcher R, Nguyen Quoc S, Davi F, Charlotte F, Dorent R, Barrou B, Vernant JP, Raphael M, Levy V. Identification of prognostic factors in 61 patients with posttransplantation lymphoproliferative disorders. J Clin Oncol. 2001 Feb 1;19(3):772-8. doi: 10.1200/JCO.2001.19.3.772. PMID: 11157030.
- Maecker B, Jack T, Zimmermann M, Abdul-Khaliq H, Burdelski M, Fuchs A, Hoyer P, Koepf S, Kraemer U, Laube GF, Müller-Wiefel DE, Netz H, Pohl M, Toenshoff B, Wagner HJ, Wallot M, Welte K, Melter M, Offner G, Klein C. CNS or bone marrow involvement as risk factors for poor survival in post-transplantation lymphoproliferative disorders in children after solid organ transplantation. J Clin Oncol. 2007 Nov 1;25(31):4902-8. doi: 10.1200/JCO.2006.10.2392. PMID: 17971586.
- Nalesnik MA. Clinicopathologic characteristics of post-transplant lymphoproliferative disorders. Recent Results Cancer Res. 2002;159:9-18. doi: 10.1007/978-3-642-56352-2_2. PMID: 11785849.
- Burns DM, Crawford DH. Epstein-Barr virus-specific cytotoxic T-lymphocytes for adoptive immunotherapy of post-transplant lymphoproliferative disease. Blood Rev. 2004 Sep;18(3):193-209. doi: 10.1016/j.blre.2003.12.002. PMID: 15183903.
- Feng S, Buell JF, Chari RS, DiMaio JM, Hanto DW. Tumors and transplantation: The 2003 Third Annual ASTS State-of-the-Art Winter Symposium. Am J Transplant. 2003 Dec;3(12):1481-7. doi: 10.1046/j.1600-6143.2003.00245.x. PMID: 14629278.
- Boubenider S, Hiesse C, Goupy C, Kriaa F, Marchand S, Charpentier B. Incidence and consequences of post-transplantation lymphoproliferative disorders. J Nephrol. 1997 May-Jun;10(3):136-45. PMID: 9238621.
- Castellano-Sanchez AA, Li S, Qian J, Lagoo A, Weir E, Brat DJ. Primary central nervous system posttransplant lymphoproliferative disorders. Am J Clin Pathol. 2004 Feb;121(2):246-53. doi: 10.1309/N82C-TQ1J-0XEV-EFQB. PMID: 14983939.
- Phan TG, O'Neill BP, Kurtin PJ. Posttransplant primary CNS lymphoma. Neuro Oncol. 2000 Oct;2(4):229-38. doi: 10.1093/neuonc/2.4.229. PMID: 11265232; PMCID: PMC1920594.
- Morton M, Coupes B, Roberts SA, Klapper PE, Byers RJ, Vallely PJ, Ryan K, Picton ML. Epidemiology of posttransplantation lymphoproliferative disorder in adult renal transplant recipients. Transplantation. 2013 Feb 15;95(3):470-8. doi: 10.1097/TP.0b013e318276a237. PMID: 23222821.
- Choquet S, Leblond V, Herbrecht R, Socié G, Stoppa AM, Vandenberghe P, Fischer A, Morschhauser F, Salles G, Feremans W, Vilmer E, Peraldi MN, Lang P, Lebranchu Y, Oksenhendler E, Garnier JL, Lamy T, Jaccard A, Ferrant A, Offner F, Hermine O, Moreau A, Fafi-Kremer S, Morand P, Chatenoud L, Berriot-Varoqueaux N, Bergougnoux L, Milpied N. Efficacy and safety of rituximab in B-cell post-transplantation lymphoproliferative disorders: results of a prospective multicenter phase 2 study. Blood. 2006 Apr 15;107(8):3053-7. doi: 10.1182/blood-2005-01-0377. Epub 2005 Oct 27. PMID: 16254143.
- González-Barca E, Domingo-Domenech E, Capote FJ, Gómez-Codina J, Salar A, Bailen A, Ribera JM, López A, Briones J, Muñoz A, Encuentra M, de Sevilla AF; GEL/TAMO (Grupo Español de Linfomas); GELCAB (Grupo para el Estudio de los Linfomas Catalano-Balear); GOTEL (Grupo Oncológico para el Tratamiento y Estudio de los Linfomas). Prospective phase II trial of extended treatment with rituximab in patients with B-cell post-transplant lymphoproliferative disease. Haematologica. 2007 Nov;92(11):1489-94. doi: 10.3324/haematol.11360. PMID: 18024397.
- Oton AB, Wang H, Leleu X, Melhem MF, George D, Lacasce A, Foon K, Ghobrial IM. Clinical and pathological prognostic markers for survival in adult patients with post-transplant lymphoproliferative disorders in solid transplant. Leuk Lymphoma. 2008 Sep;49(9):1738-44. doi: 10.1080/10428190802239162. PMID: 18798108.
- Leblond V, Sutton L, Dorent R, Davi F, Bitker MO, Gabarre J, Charlotte F, Ghoussoub JJ, Fourcade C, Fischer A, et al. Lymphoproliferative disorders after organ transplantation: a report of 24 cases observed in a single center. J Clin Oncol. 1995 Apr;13(4):961-8. doi: 10.1200/JCO.1995.13.4.961. PMID: 7707124.
- Newell KA, Alonso EM, Whitington PF, Bruce DS, Millis JM, Piper JB, Woodle ES, Kelly SM, Koeppen H, Hart J, Rubin CM, Thistlethwaite JR Jr. Posttransplant lymphoproliferative disease in pediatric liver transplantation. Interplay between primary Epstein-Barr virus infection and immunosuppression. Transplantation. 1996 Aug 15;62(3):370-5. doi: 10.1097/00007890-199608150-00012. PMID: 8779685.
- Jagadeesh D, Woda BA, Draper J, Evens AM. Post transplant lymphoproliferative disorders: risk, classification, and therapeutic recommendations. Curr Treat Options Oncol. 2012 Mar;13(1):122-36. doi: 10.1007/s11864-011-0177-x. PMID: 22241590.
- Knight JS, Tsodikov A, Cibrik DM, Ross CW, Kaminski MS, Blayney DW. Lymphoma after solid organ transplantation: risk, response to therapy, and survival at a transplantation center. J Clin Oncol. 2009 Jul 10;27(20):3354-62. doi: 10.1200/JCO.2008.20.0857. Epub 2009 May 18. PMID: 19451438.
- Elstrom RL, Andreadis C, Aqui NA, Ahya VN, Bloom RD, Brozena SC, Olthoff KM, Schuster SJ, Nasta SD, Stadtmauer EA, Tsai DE. Treatment of PTLD with rituximab or chemotherapy. Am J Transplant. 2006 Mar;6(3):569-76. doi: 10.1111/j.1600-6143.2005.01211.x. PMID: 16468968.
- Opelz G, Daniel V, Naujokat C, Döhler B. Epidemiology of pretransplant EBV and CMV serostatus in relation to posttransplant non-Hodgkin lymphoma. Transplantation. 2009 Oct 27;88(8):962-7. doi: 10.1097/TP.0b013e3181b9692d. PMID: 19855238.
- Caillard S, Dharnidharka V, Agodoa L, Bohen E, Abbott K. Posttransplant lymphoproliferative disorders after renal transplantation in the United States in era of modern immunosuppression. Transplantation. 2005 Nov 15;80(9):1233-43. doi: 10.1097/01.tp.0000179639.98338.39. PMID: 16314791.
- Valencia-Sanchez C, Steenerson KK, Kelemen K, Orenstein R, Kusne S, Grill MF. Post-transplant primary central nervous system lymphoma after Epstein-Barr virus cerebellitis. J Neurovirol. 2019 Apr;25(2):280-283. doi: 10.1007/s13365-018-0711-8. Epub 2019 Jan 3. PMID: 30607891.
- Dharnidharka VR, Webster AC, Martinez OM, Preiksaitis JK, Leblond V, Choquet S. Post-transplant lymphoproliferative disorders. Nat Rev Dis Primers. 2016 Jan 28;2:15088. doi: 10.1038/nrdp.2015.88. PMID: 27189056.
- Gupta D, Mendonca S, Chakraborty S, Chatterjee T. Post Transplant Lymphoproliferative Disorder. Indian J Hematol Blood Transfus. 2020 Apr;36(2):229-237. doi: 10.1007/s12288-019-01182-x. Epub 2019 Sep 17. PMID: 32425371; PMCID: PMC7229077.
- Velvet AJJ, Bhutani S, Papachristos S, Dwivedi R, Picton M, Augustine T, Morton M. A single-center experience of post-transplant lymphomas involving the central nervous system with a review of current literature. Oncotarget. 2019 Jan 11;10(4):437-448. doi: 10.18632/oncotarget.26522. PMID: 30728897; PMCID: PMC6355190.
- Xu QS, Ye S, Zhou YQ, Sheng JF, Ye K, Zheng SS. Posttransplantation lymphoproliferative disorder involving the central nervous system in liver transplant recipients. Hepatobiliary Pancreat Dis Int. 2008 Oct;7(5):551-4. PMID: 18842507.
- White ML, Moore DW, Zhang Y, Mark KD, Greiner TC, Bierman PJ. Primary central nervous system post-transplant lymphoproliferative disorders: the spectrum of imaging appearances and differential. Insights Imaging. 2019 Apr 11;10(1):46. doi: 10.1186/s13244-019-0726-6. PMID: 30972513; PMCID: PMC6458224.
- Lake W, Chang JE, Kennedy T, Morgan A, Salamat S, Başkaya MK. A case series of primary central nervous system posttransplantation lymphoproliferative disorder: imaging and clinical characteristics. Neurosurgery. 2013 Jun;72(6):960-70; discussion 970. doi: 10.1227/NEU.0b013e31828cf619. PMID: 23685504; PMCID: PMC4442016.
- Snanoudj R, Durrbach A, Leblond V, Caillard S, Hurault De Ligny B, Noel C, Rondeau E, Moulin B, Mamzer-Bruneel MF, Lacroix C, Charpentier B. Primary brain lymphomas after kidney transplantation: presentation and outcome. Transplantation. 2003 Sep 27;76(6):930-7. doi: 10.1097/01.TP.0000079253.06061.52. PMID: 14508356.
- Evens AM, Choquet S, Kroll-Desrosiers AR, Jagadeesh D, Smith SM, Morschhauser F, Leblond V, Roy R, Barton B, Gordon LI, Gandhi MK, Dierickx D, Schiff D, Habermann TM, Trappe R. Primary CNS posttransplant lymphoproliferative disease (PTLD): an international report of 84 cases in the modern era. Am J Transplant. 2013 Jun;13(6):1512-22. doi: 10.1111/ajt.12211. PMID: 23721553.
- Twombley K, Pokala H, Ardura MI, Harker-Murray P, Johnson-Welch SF, Weinberg A, Seikaly M. Intraventricular rituximab and systemic chemotherapy for treatment of central nervous system post-transplant lymphoproliferative disorder after kidney transplantation. Pediatr Transplant. 2012 Sep;16(6):E201-9. doi: 10.1111/j.1399-3046.2012.01699.x. Epub 2012 May 30. PMID: 22646132.
- Swerdlow SH (2017) World Health Organization. WHO classification of tumours of haematopoietic and lymphoid tissues. 5th, Lyon, France: International Agency for Research on Cancer. International Agency for Research on Cancer
- Starzl TE, Nalesnik MA, Porter KA, Ho M, Iwatsuki S, Griffith BP, Rosenthal JT, Hakala TR, Shaw BW Jr, Hardesty RL, et al. Reversibility of lymphomas and lymphoproliferative lesions developing under cyclosporin-steroid therapy. Lancet. 1984 Mar 17;1(8377):583-7. doi: 10.1016/s0140-6736(84)90994-2. PMID: 6142304; PMCID: PMC2987704.
- Reshef R, Vardhanabhuti S, Luskin MR, Heitjan DF, Hadjiliadis D, Goral S, Krok KL, Goldberg LR, Porter DL, Stadtmauer EA, Tsai DE. Reduction of immunosuppression as initial therapy for posttransplantation lymphoproliferative disorder(★). Am J Transplant. 2011 Feb;11(2):336-47. doi: 10.1111/j.1600-6143.2010.03387.x. Epub 2011 Jan 10. PMID: 21219573; PMCID: PMC3079420.
- Tsai DE, Hardy CL, Tomaszewski JE, Kotloff RM, Oltoff KM, Somer BG, Schuster SJ, Porter DL, Montone KT, Stadtmauer EA. Reduction in immunosuppression as initial therapy for posttransplant lymphoproliferative disorder: analysis of prognostic variables and long-term follow-up of 42 adult patients. Transplantation. 2001 Apr 27;71(8):1076-88. doi: 10.1097/00007890-200104270-00012. PMID: 11374406.
- Lim WH, Russ GR, Coates PT. Review of Epstein-Barr virus and post-transplant lymphoproliferative disorder post-solid organ transplantation. Nephrology (Carlton). 2006 Aug;11(4):355-66. doi: 10.1111/j.1440-1797.2006.00596.x. PMID: 16889577.
- Schultz C, Scott C, Sherman W, Donahue B, Fields J, Murray K, Fisher B, Abrams R, Meis-Kindblom J. Preirradiation chemotherapy with cyclophosphamide, doxorubicin, vincristine, and dexamethasone for primary CNS lymphomas: initial report of radiation therapy oncology group protocol 88-06. J Clin Oncol. 1996 Feb;14(2):556-64. doi: 10.1200/JCO.1996.14.2.556. PMID: 8636771.
- Mead GM, Bleehen NM, Gregor A, Bullimore J, Shirley D, Rampling RP, Trevor J, Glaser MG, Lantos P, Ironside JW, Moss TH, Brada M, Whaley JB, Stenning SP. A medical research council randomized trial in patients with primary cerebral non-Hodgkin lymphoma: cerebral radiotherapy with and without cyclophosphamide, doxorubicin, vincristine, and prednisone chemotherapy. Cancer. 2000 Sep 15;89(6):1359-70. PMID: 11002232.
- Nabors LB, Palmer CA, Julian BA, Przekwas AM, Kew CE. Isolated central nervous system posttransplant lymphoproliferative disorder treated with high-dose intravenous methotrexate. Am J Transplant. 2009 May;9(5):1243-8. doi: 10.1111/j.1600-6143.2009.02598.x. PMID: 19422350.
- Ferreri AJ, Reni M, Foppoli M, Martelli M, Pangalis GA, Frezzato M, Cabras MG, Fabbri A, Corazzelli G, Ilariucci F, Rossi G, Soffietti R, Stelitano C, Vallisa D, Zaja F, Zoppegno L, Aondio GM, Avvisati G, Balzarotti M, Brandes AA, Fajardo J, Gomez H, Guarini A, Pinotti G, Rigacci L, Uhlmann C, Picozzi P, Vezzulli P, Ponzoni M, Zucca E, Caligaris-Cappio F, Cavalli F; International Extranodal Lymphoma Study Group (IELSG). High-dose cytarabine plus high-dose methotrexate versus high-dose methotrexate alone in patients with primary CNS lymphoma: a randomised phase 2 trial. Lancet. 2009 Oct 31;374(9700):1512-20. doi: 10.1016/S0140-6736(09)61416-1. Epub 2009 Sep 18. PMID: 19767089.
- Löw S, Han CH, Batchelor TT. Primary central nervous system lymphoma. Ther Adv Neurol Disord. 2018 Oct 5;11:1756286418793562. doi: 10.1177/1756286418793562. PMID: 30305848; PMCID: PMC6174646.
- Nabors LB, Palmer CA, Julian BA, Przekwas AM, Kew CE. Isolated central nervous system posttransplant lymphoproliferative disorder treated with high-dose intravenous methotrexate. Am J Transplant. 2009 May;9(5):1243-8. doi: 10.1111/j.1600-6143.2009.02598.x. PMID: 19422350.
- Patrick A, Wee A, Hedderman A, Wilson D, Weiss J, Govani M. High-dose intravenous rituximab for multifocal, monomorphic primary central nervous system posttransplant lymphoproliferative disorder. J Neurooncol. 2011 Jul;103(3):739-43. doi: 10.1007/s11060-010-0425-0. Epub 2010 Sep 26. PMID: 20872273.
- Czyzewski K, Styczynski J, Krenska A, Debski R, Zajac-Spychala O, Wachowiak J, Wysocki M. Intrathecal therapy with rituximab in central nervous system involvement of post-transplant lymphoproliferative disorder. Leuk Lymphoma. 2013 Mar;54(3):503-6. doi: 10.3109/10428194.2012.718342. Epub 2012 Aug 31. PMID: 22873830.
- Green M, Michaels MG, Webber SA, Rowe D, Reyes J. The management of Epstein-Barr virus associated post-transplant lymphoproliferative disorders in pediatric solid-organ transplant recipients. Pediatr Transplant. 1999 Nov;3(4):271-81. doi: 10.1034/j.1399-3046.1999.00066.x. PMID: 10562971.
- Caillard S, Porcher R, Provot F, Dantal J, Choquet S, Durrbach A, Morelon E, Moal V, Janbon B, Alamartine E, Pouteil Noble C, Morel D, Kamar N, Buchler M, Mamzer MF, Peraldi MN, Hiesse C, Renoult E, Toupance O, Rerolle JP, Delmas S, Lang P, Lebranchu Y, Heng AE, Rebibou JM, Mousson C, Glotz D, Rivalan J, Thierry A, Etienne I, Moal MC, Albano L, Subra JF, Ouali N, Westeel PF, Delahousse M, Genin R, Hurault de Ligny B, Moulin B. Post-transplantation lymphoproliferative disorder after kidney transplantation: report of a nationwide French registry and the development of a new prognostic score. J Clin Oncol. 2013 Apr 1;31(10):1302-9. doi: 10.1200/JCO.2012.43.2344. Epub 2013 Feb 19. PMID: 23423742.
Figures:
Similar Articles
-
The Risk-Adjusted Impact of Intraoperative Hemofiltration on Real-World Outcomes of Patients Undergoing Cardiac SurgeryMatata BM*,Shaw M. The Risk-Adjusted Impact of Intraoperative Hemofiltration on Real-World Outcomes of Patients Undergoing Cardiac Surgery. . 2017 doi: 10.29328/journal.jcn.1001001; 1: 001-010
-
Cardiac Manifestations on Anti-Phospholipid SyndromeFaisal AH*. Cardiac Manifestations on Anti-Phospholipid Syndrome. . 2017 doi: 10.29328/journal.jcn.1001002; 1: 011-013
-
Intraperitoneal and Subsequent Intravenous Vancomycin: An Effective Treatment Option for Gram-Positive Peritonitis in Peritoneal DialysisBarone RJ*,Gimenez NS,Ramirez L. Intraperitoneal and Subsequent Intravenous Vancomycin: An Effective Treatment Option for Gram-Positive Peritonitis in Peritoneal Dialysis. . 2017 doi: 10.29328/journal.jcn.1001003; 1: 014-018
-
Acute Tubulointerstitial Nephritis due to Phenytoin: Case ReportNilzete Liberato Bresolin*,Pedro Docusse Junior,Maria Beatriz Cacese Shiozawa,Marina Ratier de Brito Moreira,Natalia Galbiatti Silveira. Acute Tubulointerstitial Nephritis due to Phenytoin: Case Report. . 2017 doi: 10.29328/journal.jcn.1001004; 1: 019-025
-
Profile of vitamin D receptor polymorphism Bsm I and FokI in end stage renal disease Egyptian patients on maintenance hemodialysisEL-Attar HA*,Mokhtar MM,Gaber EW. Profile of vitamin D receptor polymorphism Bsm I and FokI in end stage renal disease Egyptian patients on maintenance hemodialysis. . 2017 doi: 10.29328/journal.jcn.1001005; 1: 026-040
-
Anemia response to Methoxy Polyethylene Glycol-Epoetin Beta (Mircera) versus Epoetin Alfa (Eprex) in patients with chronic Kidney disease on HemodialysisAlaa K Dhayef*,Jawad K Manuti,Abdulwahab S Abutabiekh. Anemia response to Methoxy Polyethylene Glycol-Epoetin Beta (Mircera) versus Epoetin Alfa (Eprex) in patients with chronic Kidney disease on Hemodialysis. . 2017 doi: 10.29328/journal.jcn.1001006; 1: 041-047
-
The outcome of Acute Kidney Injury in patients with severe MalariaJoão Egidio Romão Jr*,João Alberto Brandão. The outcome of Acute Kidney Injury in patients with severe Malaria. . 2017 doi: 10.29328/journal.jcn.1001007; 1: 048-054
-
Short term effect of Intravenous Intermittent Iron Infusion versus Bolus Iron Infusion on Iron parameters in Hemodialysis patientsIman Ibrahim Sarhan,Hussein Sayed Hussein,Islam Omar Elshazly*,Mahmoud Salah Hassan. Short term effect of Intravenous Intermittent Iron Infusion versus Bolus Iron Infusion on Iron parameters in Hemodialysis patients. . 2017 doi: 10.29328/journal.jcn.1001008; 1: 055-059
-
Association between bh4/bh2 ratio and Albuminuria in Hypertensive Type -2 Diabetic patientsJose Aviles-Herrera,Karla C Arana-Pazos,Leonardo Del Valle-Mondragon,Carolina Guerrero-García,Alberto Francisco Rubio-Guerra*. Association between bh4/bh2 ratio and Albuminuria in Hypertensive Type -2 Diabetic patients. . 2017 doi: 10.29328/journal.jcn.1001009; 1: 060-063
-
Posterior Reversible Leukoencephalopathy Syndrome in a patient after second dose of Rituximab for treatment of resistant Thrombotic Thrombocytopenic PurpuraSabaa Asif*,Sumbal Nasir Mahmood,Osama Kunwer Naveed. Posterior Reversible Leukoencephalopathy Syndrome in a patient after second dose of Rituximab for treatment of resistant Thrombotic Thrombocytopenic Purpura . . 2018 doi: 10.29328/journal.jcn.1001010; 2: 001-004
Recently Viewed
-
Pattern of Eye Disease in Nenwe Rural Eye Clinic, Nigeria: A Seven Year ReviewNnenna Maureen Ozioko*, Nkiru Mary Okoloagu, Emmanuel Sunday Onah, Catherine. Pattern of Eye Disease in Nenwe Rural Eye Clinic, Nigeria: A Seven Year Review. Int J Clin Exp Ophthalmol. 2024: doi: 10.29328/journal.ijceo.1001056; 8: 004-015
-
Retinopathy of prematurity - Intersibling divergence of risk factors among twinsSudeep Navule Siddappa*,Kavitha Chikknayakanahalli Venugopal,Pavana Acharya ,Tintu Susan Joy . Retinopathy of prematurity - Intersibling divergence of risk factors among twins. Int J Clin Exp Ophthalmol. 2020: doi: 10.29328/journal.ijceo.1001026; 4: 009-011
-
Effectiveness of levocetirizine in treating allergic rhinitis while retaining work efficiencyDabholkar Yogesh, Shah Tanush, Rathod Roheet, Paspulate Akhila, Veligandla Krishna Chaitanya, Rathod Rahul, Devesh Kumar Joshi*, Kotak Bhavesh. Effectiveness of levocetirizine in treating allergic rhinitis while retaining work efficiency. Arch Asthma Allergy Immunol. 2023: doi: 10.29328/journal.aaai.1001031; 7: 005-011
-
Hepatic Pseudolymphoma Mimicking Neoplasia in Primary Biliary Cholangitis: A Case ReportJeremy Hassoun,Aurélie Bornand,Alexis Ricoeur,Giulia Magini,Nicolas Goossens,Laurent Spahr*. Hepatic Pseudolymphoma Mimicking Neoplasia in Primary Biliary Cholangitis: A Case Report. Arch Case Rep. 2024: doi: 10.29328/journal.acr.1001115; 8: 152-155
-
Other Applications of Amniotic Membranes: Case SeriesLinda Guerrero*. Other Applications of Amniotic Membranes: Case Series. Arch Case Rep. 2024: doi: 10.29328/journal.acr.1001117; 8: 159-162
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."