More Information
Submitted: December 26, 2022 | Approved: January 04, 2023 | Published: January 05, 2023
How to cite this article: Asiri AH, AlQarni MA, Bafaqeeh MS, Altalhi AM, Alshathri AA, et al. Complications of ultrasound-guided percutaneous native kidney biopsies in children: A single center experience. J Clini Nephrol. 2023; 7: 007-011.
DOI: 10.29328/journal.jcn.1001101
Copyright License: © 2023 Asiri AH, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Ultrasound-guided renal biopsy; Ultrasound guided kidney biopsy; Children; Complications; Indications; Prevalence; Risk factors
Complications of ultrasound-guided percutaneous native kidney biopsies in children: A single center experience
Ali H Asiri1* , Musaed A AlQarni2, Mohammed S Bafaqeeh1, Abdulhadi M Altalhi1, Abdulaziz A Alshathri1 and Khalid A Alsaran1
, Musaed A AlQarni2, Mohammed S Bafaqeeh1, Abdulhadi M Altalhi1, Abdulaziz A Alshathri1 and Khalid A Alsaran1
1Department of Pediatric Nephrology, King Saud Medical City, Riyadh, Saudi Arabia
2Department of Pediatric Nephrology, Khamis Mushait Maternity and Children Hospital, Asir, Saudi Arabia
*Address for Correspondence: Dr. Ali H Asiri, MBBS, SBP, SFPN, Pediatric Nephrology Department, Pediatric Hospital, King Saud Medical City, Al Imam Abdul Aziz Ibn Muhammad Ibn Saud, Ulaishah, Riyadh 12746, Saudi Arabia, Email: [email protected]
Introduction: Percutaneous kidney biopsy is a necessary tool to diagnose many kidney diseases. However, major complications were reported in adults, including bleeding in the kidney or around it, creation of arteriovenous fistula, wound infection, damage to adjacent organs, or even loss of the kidney. Such complications can rapidly develop serious consequences. Exploring risk factors might help in preventing them.
Objective: The current study aims to evaluate and explore the complications that happened after percutaneous kidney biopsy in children and associated risk factors.
Methodology: A retrospective record-based study was conducted by reviewing the medical records of children with post-ultrasound-guided percutaneous kidney biopsy complications at King Saud Medical City, a tertiary hospital in Riyadh, Saudi Arabia during the period from May 2014 to June 2021. Data were extracted using pre-structured data collection sheet. Data collected included children’s age, gender, primary disease, laboratory findings, and kidney complications with needed management.
Results: The study identified 76 children who had undergone 86 ultrasound-guided percutaneous kidney biopsies in the study period and fulfil the inclusion criteria. Children’s ages ranged from 1 years to 15 years with a mean age of 7.3 ± 4.0 years old. Most of the study children had nephrotic syndrome (61.6%; 53), followed by glomerulonephritis (25.6%; 22). Thirty-five (40.7%) children developed at least one of the complications. The most-reported complication was microscopic haematuria (32.6%; 28), followed by gross haematuria (3.5%; 3), Flank pain was reported among 3 (3.5%) children also and hematoma (1 child), only 2 children (3.9%) among those who had no complications recorded Haemoglobin drop > 2 g/dl compared to 3 of those who had complications with no statistical significance (p = .365). Prothrombin time was significantly higher among children who had renal complications than others who had not (11.7 ± 1.8 vs. 10.8 ± 1.2 seconds; p = .022).
Conclusion: Suggestive by the low need to intervene in complications, ultrasound-guided percutaneous kidney biopsy is a relatively safe procedure in children. Even in the most commonly observed complication, i.e. hemorrhagic ones, blood transfusion is rarely needed.
Primary and secondary kidney disease among children probably causes very severe complications or even death [1]. Mapping the etiologic field of pediatric kidney diseases is vital for both treatment and prognosis [2]. The etiology of pediatric renal diseases is mainly primary with difficulty in diagnosis using laboratory studies alone [3]. Kidney biopsy of native kidneys was presented in the 1950’s by Iversen and Brun [4]. Which was modified by Kark and Muehrcke [5]. During the previous 6 decades, renal biopsy has been an essential part of clinical practice and research in nephrology. Enhancements in imaging techniques and biopsy needles played a significant role in the capability to get adequate kidney tissue for diagnosis in more than 99% of kidney biopsies [6-8]. Moreover, these technical improvements resulted in better safety of the technique, with the lowered frequency of life-threatening complications with the decreased death rate from 0.12% to 0.02% over the past 60 years [6-12]. Recently, percutaneous kidney biopsy of native kidneys associated with death rate has been a tremendously occasional event [13]. Most of the reported complications resolve spontaneously without the need for additional management; though, the complication can be serious and hypothetically life-threatening in about 9% of biopsies, resulting in the need for intervention [12-14].
We aimed to explore the complications and risk factors for that child in King Saud Medical City, a tertiary hospital in Riyadh, which is the capital of the Kingdom of Saudi Arabia. The study site receives referrals from all over the kingdom.
A retrospective record-based study was conducted by reviewing the medical records of children with post-ultrasound-guided kidney biopsy complications at King Saud Medical City in Riyadh, Saudi Arabia, during the period from May 2014 to June 2021. All children aged 15 years or less with complete medical files were included while medical files with missing relevant data were excluded. Data were extracted using pre-structured data collection sheet. Data collected included children’s age, gender, primary disease, hemoglobin pre and post-biopsy, platelets number, serum creatinine (Jaffe), serum urea, prothrombin time (PT), partial thromboplastin time (PTT), estimated glomerular filtration rate, and renal complications with needed management.
Data analysis
After data were extracted, it was revised, coded, and fed to statistical software IBM SPSS version 22(SPSS, Inc. Chicago, IL). All statistical analysis was done using two-tailed tests. A p - value less than 0.05 was statistically significant. Descriptive analysis based on frequency and percent distribution was done for all variables including children’s bio-demographic data, laboratory findings, and kidney complications. Also, frequency distribution for required medical or surgical interventions needed was done. A mean with standard deviation was used to display scale variables following normal distribution while the median was used with skewed scale variables (serum creatinine level). Cross tabulation was used to assess the distribution of children’s kidney complications by their different bio-demographic data and laboratory findings. Relations were tested using the Pearson chi-square test and exact probability test for small frequency distributions to assess the significance of categorical variables. Independent t-test and Mann-Whitney test were used for scale variables.
The study identified 76 children who had undergone 86 ultrasound-guided kidney biopsies at the study site and fulfil the inclusion criteria. Children’s ages ranged from 1 years to 15 years with a mean age of 7.3 ± 4.0 years old. Most of the study children had nephrotic syndrome (61.6%; 53), followed by glomerulonephritis (25.6%; 22). As for gender, 46 (53.5%) were females. Forty-one (47.6%) children had a blood pressure percentile of 95% or above, according to the American Academy of Pediatrics 2017 Guideline [15]. The mean systolic blood pressure was 111.5 mmHg ± 12.0 mmHg and the mean diastolic blood pressure was 69.0 mmHg ± 9.0 mmHg.
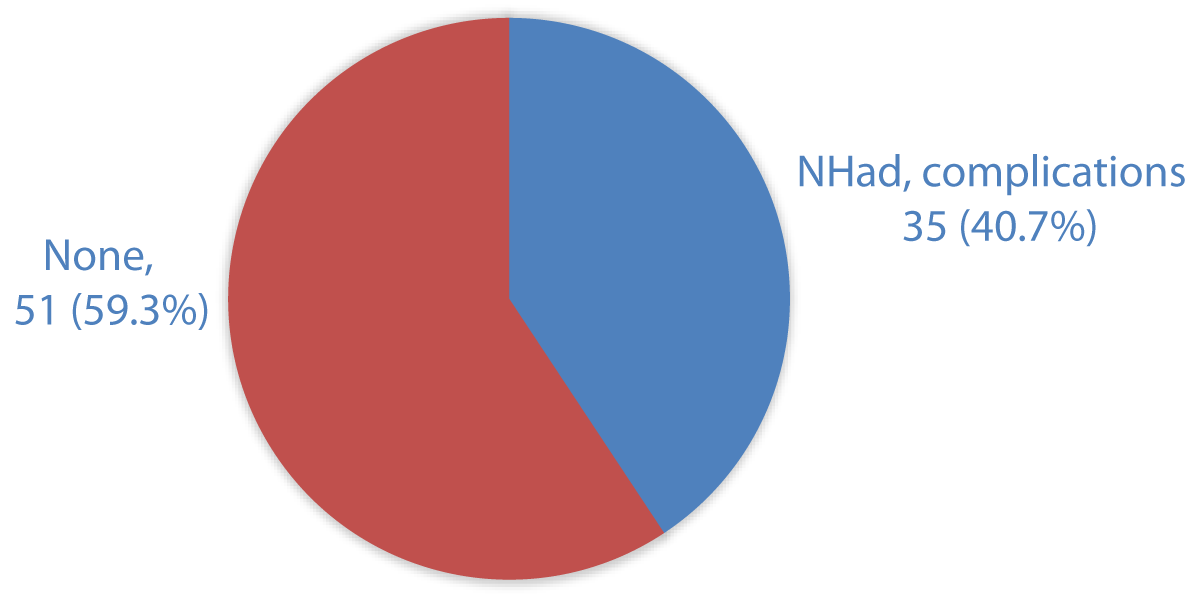
Regarding the prevalence of complications after ultrasound-guided kidney biopsy in the study children (Figure 1), thirty-five (40.7%) children developed at least one of the complications.
Figure 1: Prevalence of complications after ultrasound-guided kidney biopsy in children.
Table 1 illustrates the distribution of complications after an ultrasound-guided kidney biopsy. The most-reported complication was microscopic haematuria (32.6%; 28), followed by gross haematuria (3.5%; 3) and hematoma (1 child), while 2 children (2.3%) had all of these complications. Flank pain was reported among 3 (3.5%) children.
| Table 1: Distribution of Complications After Ultrasound-Guided Kidney Biopsy in Children, King Saud Medical City in Riyadh, Saudi Arabia. | ||
| Complications | No | % |
| Only microscopic haematuria | 28 | 32.6% |
| Only hematoma | 1 | 1.2% |
| Gross haematuria | 3 | 3.5% |
| All of the above | 2 | 2.3% |
| Flank pain | 3 | 3.5% |
Table 2 shows the distribution of complications after ultrasound-guided kidney biopsy in Children by their bio-demographic data. As for primary disease, the most reported among children with renal complications was glomerulonephritis (48.6%) followed by nephrotic syndrome (42.9%) while nephrotic syndrome was the most common among children who had no complication (74.5%) with recorded statistical significance (p = 0.001). As for age, 54.3% of children had renal complications aged 10-15 years while 52.9% of those without complications aged 1 years - 5 years (p = 0.001). Also, 80% of children with complications were females while 64.7% of those with no complications were males (p = 0.001). The mean systolic blood pressure among children who developed renal complications was 116.2 ± 12.0 vs. 108.1 ± 10.9 for others who were free of complications (p = 0.001).
| Table 2: Distribution of complications after ultrasound-guided kidney biopsy in children by their bio-demographic data. | |||||||
| Bio-demographic data | All cases (n = 86) |
Had complications | p - value | ||||
| Yes (n = 35) |
No (n = 51) |
||||||
| No | % | No | % | No | % | ||
| Primary Disease | .001* | ||||||
| Nephrotic syndrome | 53 | 61.6% | 15 | 42.9% | 38 | 74.5% | |
| Glomerulonephritis | 22 | 25.6% | 17 | 48.6% | 5 | 9.8% | |
| Chronic Kidney Disease of unknown etiology | 5 | 5.8% | 1 | 2.9% | 4 | 7.8% | |
| Hemolytic uremic syndrome | 3 | 3.5% | 2 | 5.7% | 1 | 2.0% | |
| Transplant Rejection | 3 | 3.5% | 0 | 0.0% | 3 | 5.9% | |
| Age in years | .001* | ||||||
| 1 - 5 | 31 | 36.0% | 4 | 11.4% | 27 | 52.9% | |
| 6 - 9 | 26 | 30.2% | 12 | 34.3% | 14 | 27.5% | |
| 10 - 15 | 29 | 33.7% | 19 | 54.3% | 10 | 19.6% | |
| Gender | .001* | ||||||
| Male | 40 | 46.5% | 7 | 20.0% | 33 | 64.7% | |
| Female | 46 | 53.5% | 28 | 80.0% | 18 | 35.3% | |
| BP Centile% | .428 | ||||||
| 50th | 16 | 18.6% | 9 | 25.7% | 7 | 13.7% | |
| 90th | 29 | 33.7% | 10 | 28.6% | 19 | 37.3% | |
| 95th | 31 | 36.0% | 11 | 31.4% | 20 | 39.2% | |
| 99th | 10 | 11.6% | 5 | 14.3% | 5 | 9.8% | |
| SBP | .001*# | ||||||
| Mean ± SD | 111.5 ± 12.0 | 116.2 ± 12 | 108.1 ± 10.9 | ||||
| DBP | .320 | ||||||
| Mean ± SD | 69.0 ± 9.0 | 70.2 ± 9.4 | 68.2 ± 8.7 | ||||
| P: Pearson x2 test; #: Independent t – test; * p < 0.05 (significant) | |||||||
Table 3 shows the distribution of complications after ultrasound-guided kidney biopsy in Children by their laboratory findings. Only 2 children (3.9%) among those who had no complications recorded a Haemoglobin drop > 2 g/dl post-biopsy compared to 3 of those who had complications with no statistical significance (p = 0.365). Prothrombin time was significantly higher among children who had renal complications than others who hadn’t (11.7 ± 1.8 vs. 10.8 ± 1.2 seconds; p = 0.022). There was no significant difference regarding PTT (31.1 ± 6.8 vs. 31.3 ± 7.1; p = 0.871). Platelet was found to be less than 150,000 in 2 patients (2.3%) one of them developed a complication (p = 0.153). As for creatinine, the average level among children who developed renal complications was 65 micromoles/L in comparison to 29 micromoles/L among others (p = 0.036). Serum urea was found to be higher than 20 mmol/L in one patient for those who developed complications (p = 0.084). Estimated glomerular filtration rate < 100 ml/min was recorded among 48.6% of children with complications compared to 29.4% of others without (p = 0.071).
| Table 3: Distribution of complications after ultrasound-guided kidney biopsy in children by their laboratory findings. | ||||||||
| Laboratory investigations | All cases (n = 86) |
Had complications | p - value | |||||
| Yes (n = 35) |
No (n = 51) |
|||||||
| No | % | No | % | No | % | |||
| Hemoglobin pre (mean ± SD) mg/dl | 11.7 ± 1.8 | 11.6 ± 1.8 | 11.8 ± 1.9 | .740# | ||||
| Haemoglobin post (mean ± SD) mg/dl | 11.2 ± 2.2 | 10.9 ± 2.3 | 11.5 ± 2.1 | .281# | ||||
| Haemoglobin difference > 2 g/dl | 5 | 5.8% | 3 | 8.6% | 2 | 3.9% | .365^ | |
| Platelet < 150,000 | 2 | 2.3% | 1 | 2.8% | 1 | 2.0% | .153 | |
| PT (mean ± SD) seconds | 11.2 ± 1.6 | 11.7 ± 1.8 | 10.8 ± 1.2 | .022*# | ||||
| PT > 15 seconds | 4 | 4.7% | 3 | 8.6% | 1 | 2.0% | .153^ | |
| PTT (mean ± SD) seconds | 31.2 ± 6.9 | 31.1 ± 6.8 | 31.3 ± 7.1 | .871# | ||||
| PTT > 45 seconds | 3 | 3.5% | 0 | 0.0% | 3 | 5.9% | .144^ | |
| Serum creatinine (median) 100 micromole/L | 35 | 65 | 29 | .036*$ | ||||
| Serum creatinine > 100 micromole/L | 25 | 29.1% | 13 | 37.1% | 12 | 23.5% | .172 | |
| Urea > 20 mmol/L | 7 | 8.1% | 1 | 2.8% | 6 | 11.7% | .084 | |
| Estimated glomerular filtration rate < 100 ml/min | 32 | 37.2% | 17 | 48.6% | 15 | 29.4% | .071 | |
| P: Pearson x2 test; #: Independent t – test; $: Mann-Whitney test; * p < 0.05 (significant) | ||||||||
Regarding the management of complications (Table 4), only blood transfusion was done for 3 children (8.6%) and no surgical or radiological intervention was needed.
| Table 4: Needed management for children developed complications after ultrasound-guided kidney biopsy. | ||
| Needed management | No (35) | % |
| Blood Transfusion after complications | ||
| Yes | 3 | 8.6% |
| No | 32 | 91.4% |
| Intervention for complications | ||
| Yes | 0 | 0.0% |
| No | 35 | 100.0% |
Till now and to the best of our knowledge, published research exploring the risk factors for complications of ultrasound-guided renal biopsy in children specifically does not exist. Percutaneous ultrasound-guided kidney biopsy is considered one of the diagnostic procedures for kidney diseases, delivering significant evidence in launching the diagnosis, assessing the severity, detecting disease advance, and assessing the response to therapy [16]. Nevertheless, the technique reported major complications, such as perirenal hematoma, arteriovenous fistula, infection, damage to adjacent organs, or loss of the kidney [2,17]. In the pediatric population, these complications if neglected, can quickly turn into serious consequences.
The current study revealed that less than half of the children (41%) who had undergone renal biopsy developed renal complications. The most-reported complications were associated with bleeding circumstances including haematuria (mainly microscopic) and hematoma. Flank pain was a very rarely reported complication. These complications needed only blood transfusion for 3 children with no need for intervention. This estimated complication rate was higher than what was reported by Ding JJ, et al. [18] who estimated that the overall complication rate was 15.9%. Exactly, 3.0% had major complications and while 12.9% had minor complications. The major complications were perirenal hematoma requiring blood transfusion (4 cases, 2.0%), then perirenal abscess (1 case, 0.5%) and arteriovenous fistula (1 case, 0.5%). All patients recovered without consequences after treatment. Also, other studies estimated complications among 0.1% to 4.8% [17,19-22]. The incidence of current study children with hemorrhagic complications who needed blood transfusion was 8.6%, which is somewhat higher than that (0.2% - 2.4%) reported by Varnell, et al. [22] Also, Sun YS, et al. [23] estimated that Pediatric SLE patients reported a higher rate of major complications (12.5%) than adult patients (2.3%). Locally, Abdel-Hafez MA, et al. [24] reported a lower rate of post-renal biopsy complications among children in Saudi Arabia. The common complications were gross haematuria in three (2.8%) and severe pain at the biopsy site in 11 (10.2%). None of the patients needed blood transfusions or prolonged hospitalization.
Regarding risk factors of developing complications, the current study showed that primary disease was one of the significant predictors where most children who developed complications complained of glomerulonephritis and nephrotic syndrome (which was dominant among others with no complications). Also, old-aged children (above 10 years), females, and high systolic blood pressure were significant factors associated with developing complications. Considering laboratory findings which significantly associated with the existence of complications, prolonged PT with high serum creatinine level and low estimated glomerular filtration rate were the most significant predictors. This explains the high percentage of hemorrhagic complications among the current study patients. In reference to Varnell, et al.’s study [22], elevated serum creatinine, prolonged prothrombin and thrombocytopenia increased the overall complication risk of initial kidney biopsy which matches the current study findings.
Suggestive by the low need to intervene in complications, an ultrasound-guided percutaneous biopsy of native kidneys is a relatively safe procedure in children. Even in the most commonly observed complication, i.e. hemorrhagic ones, blood transfusion is rarely needed. Low eGFR and prolonged PT are independent risk factors for complications. Platelets of less than 150,000 and serum urea of more than 36 mmol/L were found to be at an increased risk of bleeding complications.
- McDonald SP, Craig JC; Australian and New Zealand Paediatric Nephrology Association. Long-term survival of children with end-stage renal disease. N Engl J Med. 2004 Jun 24;350(26):2654-62. doi: 10.1056/NEJMoa031643. PMID: 15215481.
- Hogan JJ, Mocanu M, Berns JS. The Native Kidney Biopsy: Update and Evidence for Best Practice. Clin J Am Soc Nephrol. 2016 Feb 5;11(2):354-62. doi: 10.2215/CJN.05750515. Epub 2015 Sep 2. PMID: 26339068; PMCID: PMC4741037.
- Santangelo L, Netti GS, Giordano P, Carbone V, Martino M, Torres DD, Rossini M, Di Palma AM, Gesualdo L, Giordano M. Indications and results of renal biopsy in children: a 36-year experience. World J Pediatr. 2018 Apr;14(2):127-133. doi: 10.1007/s12519-018-0147-5. Epub 2018 Mar 22. PMID: 29569185.
- Agarwal SK, Sethi S, Dinda AK. Basics of kidney biopsy: A nephrologist's perspective. Indian J Nephrol. 2013 Jul;23(4):243-52. doi: 10.4103/0971-4065.114462. PMID: 23960337; PMCID: PMC3741965.
- Korbet SM. Percutaneous renal biopsy. Semin Nephrol. 2002 May;22(3):254-67. doi: 10.1053/snep.2002.31713. PMID: 12012311.
- Manno C, Strippoli GF, Arnesano L, Bonifati C, Campobasso N, Gesualdo L, Schena FP. Predictors of bleeding complications in percutaneous ultrasound-guided renal biopsy. Kidney Int. 2004 Oct;66(4):1570-7. doi: 10.1111/j.1523-1755.2004.00922.x. PMID: 15458453.
- Pokhrel A, Agrawal RK, Baral A, Rajbhandari A, Hada R. Percutaneous Renal Biopsy: Comparison of Blind and Real-time Ultrasound Guided Technique. J Nepal Health Res Counc. 2018 Mar 13;16(1):66-72. PMID: 29717293.
- Pasquariello A, Innocenti M, Batini V, Pasquariello G, Beati S, Rindi S, Paoletti S, Panichi V. Theoretical calculation of optimal depth in the percutaneous native kidney biopsy to drastically reduce bleeding complications and sample inadequacy for histopathological diagnosis. Nephrol Dial Transplant. 2007 Dec;22(12):3516-20. doi: 10.1093/ndt/gfm272. Epub 2007 Sep 21. PMID: 17890249.
- Whittier WL, Korbet SM. Timing of complications in percutaneous renal biopsy. J Am Soc Nephrol. 2004 Jan;15(1):142-7. doi: 10.1097/01.asn.0000102472.37947.14. PMID: 14694166.
- Bataille S, Jourde N, Daniel L, Mondain JR, Faure M, Gobert P, Alcheikh-Hassan Z, Lankester M, Giaime P, Gaudart J, Dussol B, Berland Y, Burtey S. Comparative safety and efficiency of five percutaneous kidney biopsy approaches of native kidneys: a multicenter study. Am J Nephrol. 2012;35(5):387-93. doi: 10.1159/000337932. Epub 2012 Apr 13. PMID: 22508466.
- Carrington CP, Williams A, Griffiths DF, Riley SG, Donovan KL. Adult day-case renal biopsy: a single-centre experience. Nephrol Dial Transplant. 2011 May;26(5):1559-63. doi: 10.1093/ndt/gfq571. Epub 2010 Sep 21. PMID: 20858764.
- Hwang Y, Shin YR, Lee SL, Won YD, Ku YM. Ultrasound-Guided Percutaneous Biopsy of the Native Kidney: An Axial Approach Along Brödel Avascular Plane of the Lower Pole. Ultrasound Q. 2017 Jun;33(2):144-147. doi: 10.1097/RUQ.0000000000000289. PMID: 28481764.
- Ding JJ, Lin SH, Huang JL, Wu TW, Hsia SH, Lin JJ, Chou YC, Tseng MH. Risk factors for complications of percutaneous ultrasound-guided renal biopsy in children. Pediatr Nephrol. 2020 Feb;35(2):271-278. doi: 10.1007/s00467-019-04367-8. Epub 2019 Nov 14. PMID: 31728747.
- Schorr M, Roshanov PS, Weir MA, House AA. Frequency, Timing, and Prediction of Major Bleeding Complications From Percutaneous Renal Biopsy. Can J Kidney Health Dis. 2020 May 25;7:2054358120923527. doi: 10.1177/2054358120923527. PMID: 32547772; PMCID: PMC7251654.
- Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, de Ferranti SD, Dionne JM, Falkner B, Flinn SK, Gidding SS, Goodwin C, Leu MG, Powers ME, Rea C, Samuels J, Simasek M, Thaker VV, Urbina EM; SUBCOMMITTEE ON SCREENING AND MANAGEMENT OF HIGH BLOOD PRESSURE IN CHILDREN. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017 Sep;140(3):e20171904. doi: 10.1542/peds.2017-1904. Epub 2017 Aug 21. Erratum in: Pediatrics. 2017 Nov 30;: Erratum in: Pediatrics. 2018 Sep;142(3): PMID: 28827377.
- Haładyj E, Cervera R. Do we still need renal biopsy in lupus nephritis? Reumatologia. 2016;54(2):61-6. doi: 10.5114/reum.2016.60214. Epub 2016 Jun 3. PMID: 27407281; PMCID: PMC4918045.
- Tøndel C, Vikse BE, Bostad L, Svarstad E. Safety and complications of percutaneous kidney biopsies in 715 children and 8573 adults in Norway 1988-2010. Clin J Am Soc Nephrol. 2012 Oct;7(10):1591-7. doi: 10.2215/CJN.02150212. Epub 2012 Jul 26. PMID: 22837269; PMCID: PMC3463204.
- Ding JJ, Lin SH, Huang JL, Wu TW, Hsia SH, Lin JJ, Chou YC, Tseng MH. Risk factors for complications of percutaneous ultrasound-guided renal biopsy in children. Pediatr Nephrol. 2020 Feb;35(2):271-278. doi: 10.1007/s00467-019-04367-8. Epub 2019 Nov 14. PMID: 31728747.
- Rianthavorn P, Kerr SJ, Chiengthong K. Safety of paediatric percutaneous native kidney biopsy and factors predicting bleeding complications. Nephrology (Carlton). 2014 Mar;19(3):143-8. doi: 10.1111/nep.12184. PMID: 24313556.
- Wang C, Yang Y, Jin L, Zhang Y, Chen G, Zhou Z, Song M, Gao Q, Li C, Pan T, He F, Ma L. Evaluating renal biopsy-associated hemorrhage complications by the equation and providing an early intervention: a single-center experience. J Nephrol. 2015 Dec;28(6):691-700. doi: 10.1007/s40620-015-0197-x. Epub 2015 Apr 15. PMID: 25872664.
- Al Makdama A, Al-Akash S. Safety of percutaneous renal biopsy as an outpatient procedure in pediatric patients. Ann Saudi Med. 2006 Jul-Aug;26(4):303-5. doi: 10.5144/0256-4947.2006.303. PMID: 16883085; PMCID: PMC6074502.
- Varnell CD Jr, Stone HK, Welge JA. Bleeding Complications after Pediatric Kidney Biopsy: A Systematic Review and Meta-Analysis. Clin J Am Soc Nephrol. 2019 Jan 7;14(1):57-65. doi: 10.2215/CJN.05890518. Epub 2018 Dec 6. PMID: 30522995; PMCID: PMC6364534.
- Sun YS, Sun IT, Wang HK, Yang AH, Tsai CY, Huang CJ, Huang DF, Lai CC. Risk of complications of ultrasound-guided renal biopsy for adult and pediatric patients with systemic lupus erythematosus. Lupus. 2018 Apr;27(5):828-836. doi: 10.1177/0961203317751048. Epub 2018 Jan 4. PMID: 29301470.
- Abdel-Hafez MA, Abdel-Nabi H, El-Gamasy M, Zayton H, Nassar I. Histopathological patterns of renal diseases in egyptian children: A single-center experience. Saudi J Kidney Dis Transpl. 2017 Sep-Oct;28(5):1085-1091. doi: 10.4103/1319-2442.215139. PMID: 28937067.