More Information
Submitted: January 28, 2025 | Approved: February 07, 2025 | Published: February 10, 2025
How to cite this article: Azad P, Rizvi YS, Jha LK, Tyagi P, Rastogi V. Percutaneous Transhepatic Tunneled Dialysis Catheter For Hemodialysis Access Failure. J Clini Nephrol. 2025; 9(2): 033-036. Available from:
https://dx.doi.org/10.29328/journal.jcn.1001151
DOI: 10.29328/journal.jcn.1001151
Copyright license: © 2025 Azad P, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Hemodialysis access failure; Tunneled dialysis catheter; Transhepatic vein; End-stage renal disease
Percutaneous Transhepatic Tunneled Dialysis Catheter For Hemodialysis Access Failure
Pulak Azad1*, Yasir Sultan Rizvi1, Lakshmi Kant Jha1, Pranav Tyagi1 and Vikas Rastogi2
1Nephrology, Dharamshilla Narayana Superspeciality Hospital, Delhi-110096, India
2PDCC Interventional Nephrology, MD Radiodiagnosis, India
*Address for Correspondence: Pulak Azad, Ist year Dr. NB Resident, Nephrology, Dharamshilla Narayana Superspeciality Hospital, Delhi-110096, India, Email: azad.aditya11@gmail.com
Vascular access failure is not only a big challenge for nephrologists but also a big threat for patients on haemodialysis. Due to various causes, hemodialysis patients land eventually at this dead end. Patients who have undergone multiple surgeries have intrabdominal adhesions which makes peritoneal dialysis impossible. Such patients have two options; translumbar and transhepatic access. We report a case of a 54-year-old woman who had vascular access failure. She was obese and was apprehensive about the translumbar approach of tunneled catheter placement. The transhepatic tunneled catheter was planned and under ultrasound and fluoroscopy guidance, it was inserted. The patient is undergoing hemodialysis from this access successfully.
Haemodialysis is the commonest form of kidney replacement therapy in the world, accounting for approximately 69% of all kidney replacement therapy and 89% of all dialysis [1]. Arteriovenous fistula, arteriovenous grafts, and tunneled dialysis catheters are the conventional vascular accesses. The tunneled dialysis catheter acts as a bridge to arterio-venous fistula as it takes 2 months for a fistula to mature [2,3]. In developing countries hemodialysis is the most frequently used mode of renal replacement therapy. Common indications of haemodialysis are acute kidney injury, uremic encephalopathy, pericarditis, life-threatening hyperkalemia, refractory acidosis, hypervolemia causing end-organ complications (e.g., pulmonary edema), asymptomatic patients with a GFR of 5 to 9 mL/min/1.73 m² and toxic ingestion [4].
Common complications of securing vascular access are bleeding, thrombus formation, and infection. Smooth vascular access is imperative to ensure good blood flow and hence a good clearance. Primary diseases, ageing, infections, and other comorbidities altogether make the patient predisposed to vascular access failure [2]. Here we report one such case with multiple vascular access failure and intrabdominal adhesions making peritoneal dialysis impossible as well. In such scenarios, the trans-lumbar approach of tunneled catheter insertion is a life-saving alternative and is considered a bail-out option by various authors [3].
A 54-year-old female with a known case of type 2 diabetes, hypertension, and chronic kidney disease initiated haemodialysis in August 2018 and underwent maintenance haemodialysis twice a week. Earlier used access were arterio-venous fistulae of the left upper limbs followed by the right upper limb followed by tunneled dialysis catheters in the right jugular vein followed by the left jugular vein. Thereafter, the patient underwent tunneled dialysis catheter placement in the right femoral vein followed by the left femoral veins. Contrast-enhanced computed tomography scan and digital subtraction angiography showed thrombosis in bilateral jugular, subclavian, and femoral veins. As the patient’s vascular accesses were getting exhausted, peritoneal dialysis was planned. The patient had a history of multiple abdominal surgeries like a lower segmental caesarean section and hysterectomy. The patient underwent an attempt at peritoneal dialysis catheter insertion but the procedure was abandoned due to the presence of multiple intrabdominal adhesions. Meanwhile, the patient underwent single-lumen hemodialysis catheter insertion in the left-sided long saphenous vein in the lower limb and the left basilic vein in the left upper limb. Thus hemodialysis was continued from these acceses for a few days. However, a simultaneous plan for trans-lumbar tunneled catheter insertion was made by the treating team. The patient was uncomfortable with the fact that the dialysis access would be done from the back and was apprehensive about her being lying supine in the future. So the plan for a percutaneous trans-hepatic tunneled dialysis catheter was made.
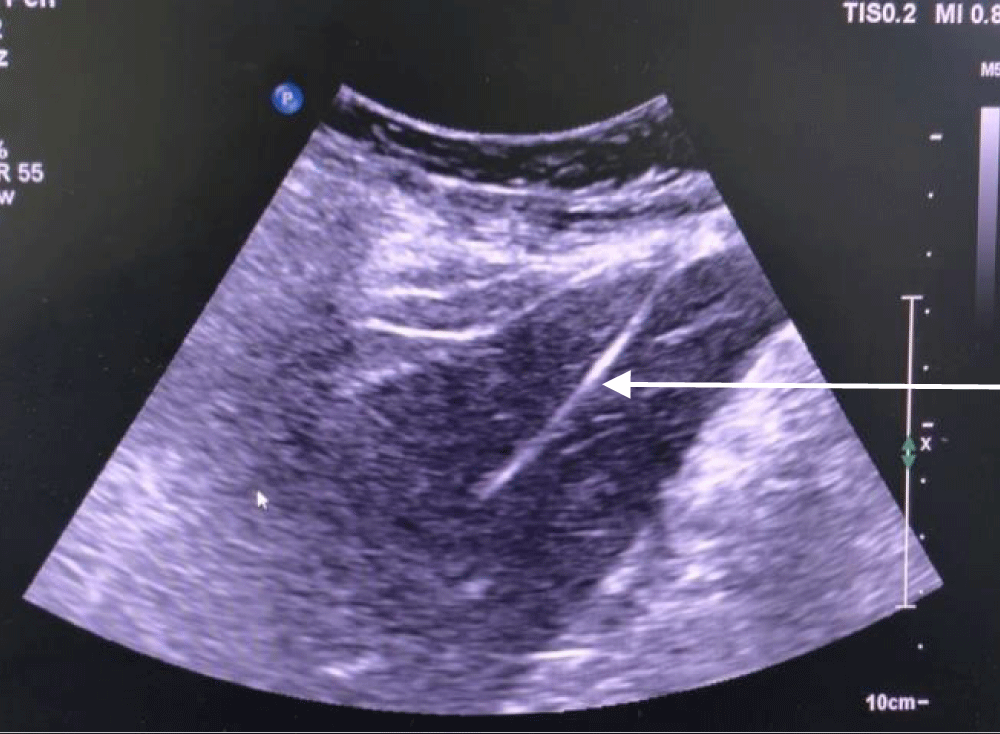
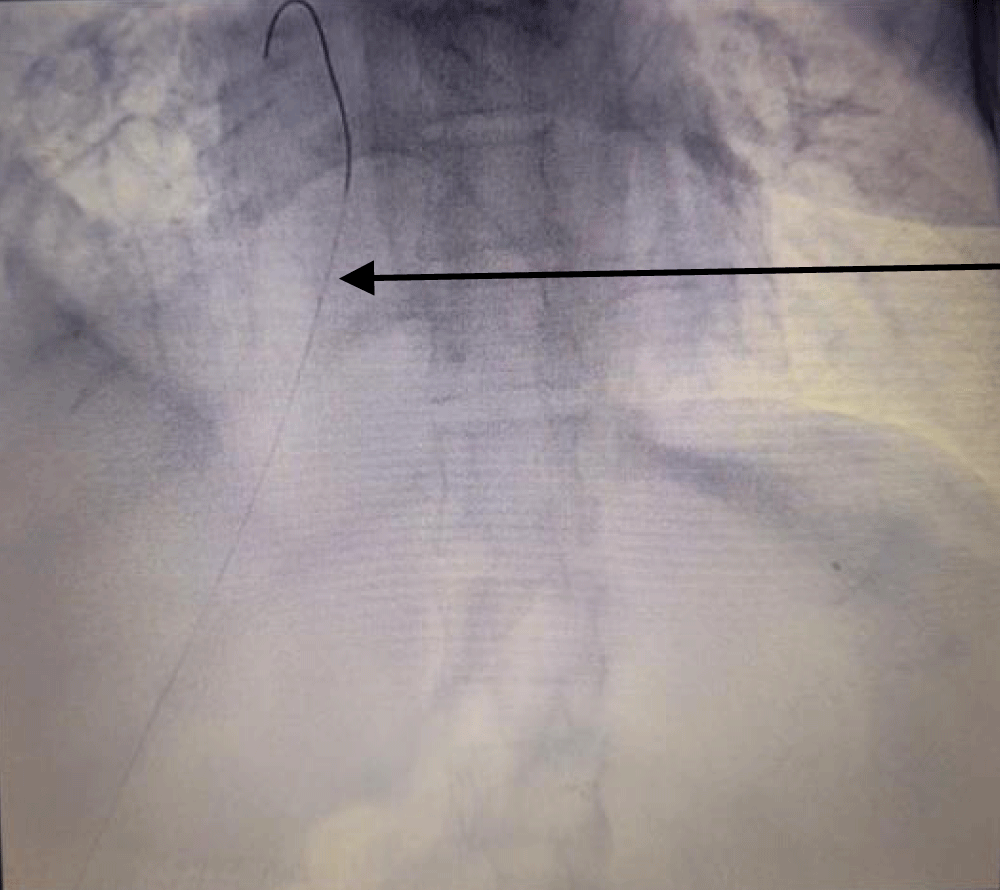
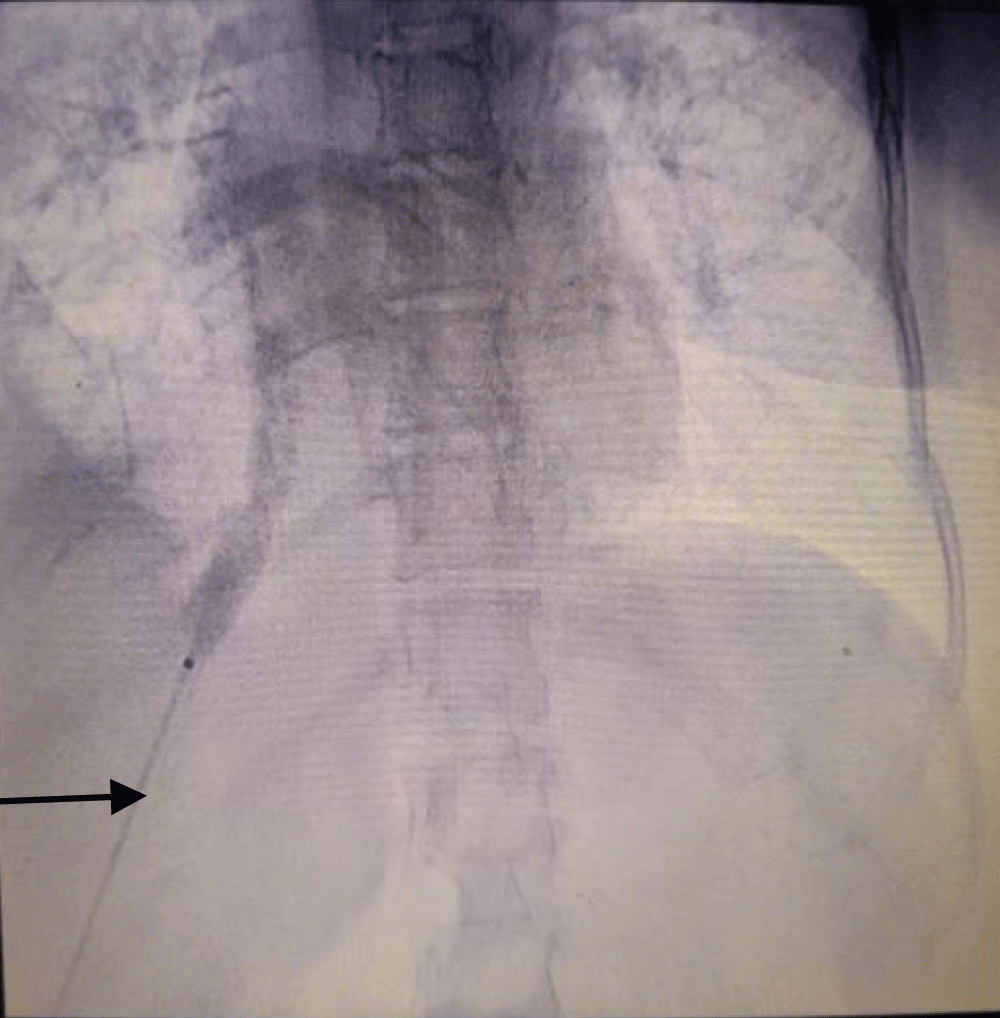
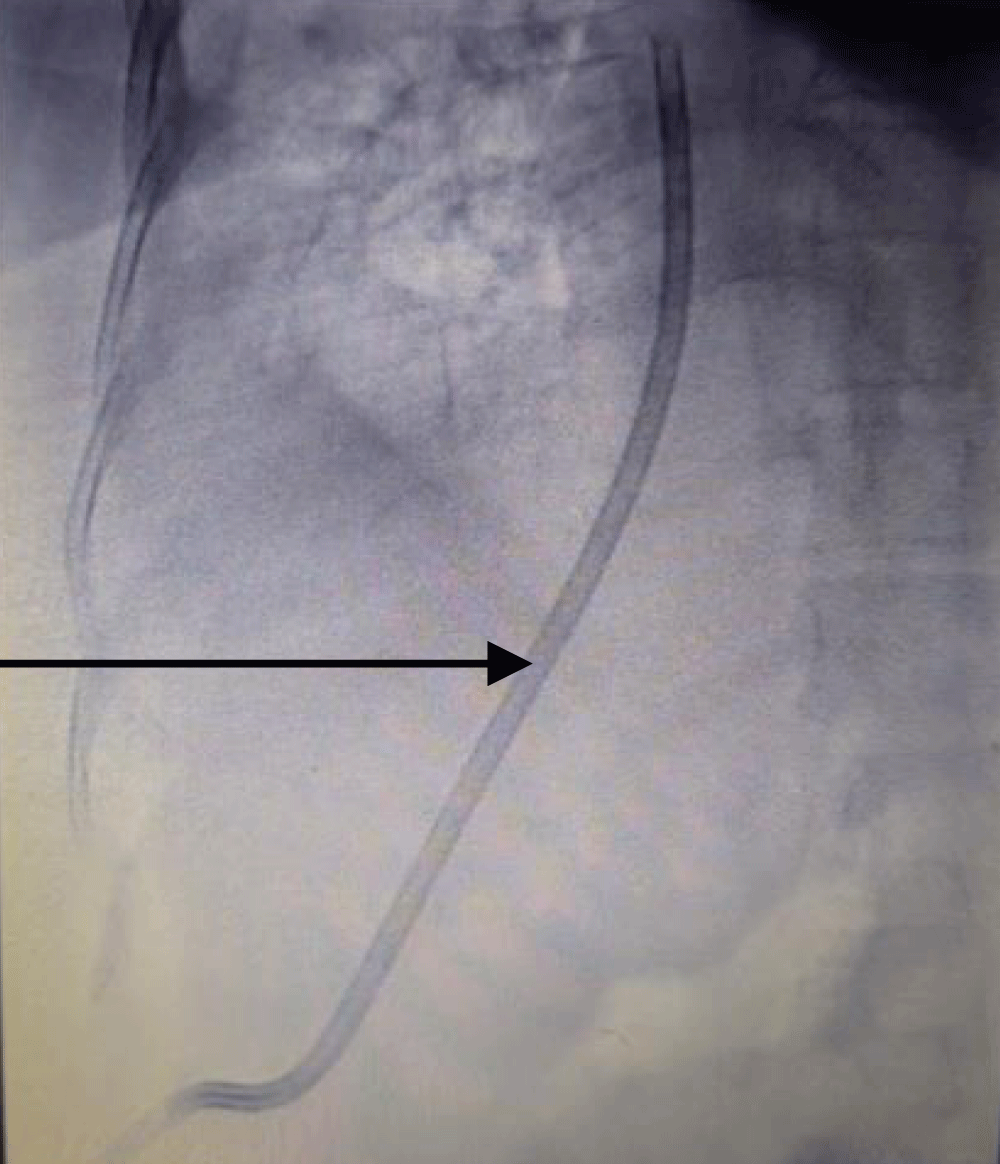
The patient was taken to the cath lab where the procedure was done under ultrasound and fluoroscopy guidance. The procedure was done with a sterile technique and using anti-septic measures; in the cath lab. After cleaning and draping the abdomen, first the right hepatic vein was visualized via ultrasound, and it was punctured by a Chiba needle via the percutaneous route. A guide wire was passed and its position was traced by ultrasound (Figure 1) and fluoroscopy (Figure 2). Radial artery sheath and Kumpe catheter were used as needed to negotiate guide wire in the inferior vena cava and right atrium. A subcutaneous tunnel of 5 cm was created and a tunnelled dialysis catheter was pulled through it (Figure 3). Contrast was injected into the sheath to visualize its flow. The contrast was seen flowing in the right atrium confirming the correct position of the sheath and the kumpe wire (Figure 4). The guide wire was then reinserted into the sheath. As the guide wire reached the inferior vena cava, it was negotiated to the right atrium. This was followed by the removal of the sheath and kumpe wire. After confirming the position of the guide wire in the right atrium (Figure 2), sequential dialation of the tract was done by dilators 6 fr, 8 fr, 10 fr, 12 fr, 14 fr, and finally 14.5 Fr x 19 cm trans-hepatic tunneled dialysis catheter was secured along with subcutaneous tunnel (Figures 5,6). The catheter tip was kept at the junction of the right atria – inferior vena cava (Figure 5). Ultrasound of the liver was done to rule out haemorrhage. There was slight post-operative pain post catheter insertion which subsided after a while. She was kept in the intensive care unit for a day for monitoring of vitals and was moved to the ward the next day. The procedure was uneventful. After being discharged, the patient underwent multiple sessions of hemodialysis with this access. She was told to take proper hygiene care of the area where the catheter was inserted to prevent catheter-related bloodstream infections. She once had an upper respiratory tract infection following which she had poor flow from the tunneled trans-hepatic dialysis catheter. She underwent repositioning of the catheter in the cath lab following which good flow was achieved. She was explained to avoid forceful coughing which can displace the catheter from its position; hampering the flow.
Figure 1: Guide wire (arrow pointing at it) traced via ultrasound in the inferior vena– cava after puncturing the right hepatic vein by Chiba needle and inserting the guide wire.
Figure 2: Fluoroscopy image of guide wire (arrow pointing at it) being negotiated from right hepatic vein to inferior vena cava and finally to right atrium.
Figure 3: Image showing a part of tunneled dialysis catheter being in a subcutaneous tunnel before final insertion.
Figure 4: Fluoroscopic image showing contrast flowing in the right atrium after being injected from the sheath(arrow pointing at it);thus confirming the correct position of sheath before final insertion of guide wire and tunneled catheter.
Figure 5: Fluoroscopic image showing trace of trans-hepatic tunneled dialysis catheter(arrow pointing at it)from right hepatic vein to inferior vena cava and then to right atrium.
Figure 6: External appearance of Trans-hepatic tunneled dialysis catheter after insertion.
Arterio-venous fistula, arterio-venous grafts, and tunneled dialysis catheters are the conventional vascular accesses. The tunneled dialysis catheter acts as a bridge to arterio-venous fistula as it takes 2 months for a fistula to mature [2,3]. The conventional used sites for placement of tunneled dialysis catheters in order of preference are the right internal jugular vein, left internal jugular vein, femoral vein, and subclavian vein. Whereas unconventional venous accesses are the external jugular vein, translumbar inferior vena cava, and hepatic vein [5]. In case of exhaustion of all conventional vascular access; a translumbar approach to the inferior vena cava is an alternative [3]. As the radius of the vein is large; thrombosis is rare, making this approach reliable [6].
Our patient was obese, apprehensive, and uncomfortable with this approach hence the plan was dropped. In comparison to the trans-lumbar approach, the trans-hepatic approach has a lesser chance of damage to the surrounding structures, and less chance of bleeding, and if occurs it is easily controlled by embolization, it is an easier approach for obese patients and even revision is easily possible [7]. The disadvantage of the trans-hepatic approach is frequent catheter migration and displacement. Even coughing or abdominal distension can cause catheter migration. This is due to the short distance between the right atrium, inferior vena cava, and hepatic vein [8,9]. In cases where there is infradiaphragmic thrombosis of the inferior vena cava, the trans-hepatic approach is preferred over the trans-lumbar [2].
The first description of transhepatic catheterization was given by Po, et al. in 1994 on an adult patient with end-stage lupus nephritis who had no alternative for vascular access and failed peritoneal dialysis; it was technically successful with no bleeding or thrombotic complications, and the patient underwent dialysis from that vascular access for a year [10]. The patency rate in the transhepatic approach in various studies has been reported from 24 days to 90 days [2]. The 36 transhepatic catheters studied by Stavropoulos, et al. reported a primary patency of just 24.3 due to a high rate of late thrombosis [11]. A study on the 127 transhepatic catheters done by Younes et al reported a much higher patency of 87.7 days [12]. However, a study done by Khallaf et al. reported a mean patency time of 280 days and a mean cumulative patency duration of 557 days. Catheter migration, sepsis, thrombosis, and exit site infection rates were 0.14, 0.15, 0.18, and 0.32 per 100 catheter-day respectively. They included 180 males and 116 females with a mean age of 53.2 years ± 11.7 years ranging from 38 to 65 years [13]. Transhepatic tunneled dialysis catheters can result in liver hemorrhage in about 29% of the cases [14]. The most common hepatic vein access by Khallaf, et al. was the right hepatic vein followed by the middle hepatic vein. The right hepatic vein is preferred as a first choice as it is peripheral (near the puncture site) as well as it obtains a horizontal upper part towards the IVC [13]. Joaquim et al. use the right hepatic vein in all cases, also El Garib et al. use either right or middle hepatic veins [15,16]. In the study done by Khallaf, et al. the tip of the hemodialysis catheter was in the right atrium (80% of cases), and in the IVC in 20% of cases [13]. This is coinciding with El Garib et al. whose catheter tip was placed in the right atrium in 80% of cases, IVC in 16% of cases, and SVC in 4% of cases [16]. Joaquim, et al. placed the catheter tip at the junction between the SVC and the right atrium in all six cases he performed [14]. In our patient, the catheter tip is at the junction of the right atria – inferior vena cava.
A-V fistulae and conventional tunneled dialysis catheters on exhaustion leading to vascular access failure seemed like a dead end for our patient. Obesity and apprehension of the translumbar approach led to the transhepatic approach of tunneled haemodialysis catheter insertion in our patient. However technically challenging it is, transhepatic tunneled dialysis catheter insertion still can provide a rescue for patients with failed haemodialysis access. Patients on haemodialysis after exhaustion of vascular access usually go for peritoneal dialysis. However, peritoneal dialysis was not possible as in our patient there was intrabdominal adhesions. One should watch for complications such as liver haemorrhage, catheter migration, displacement, exit site infection, sepsis, and thrombosis in such patients. Hence translumbar and transhepatic approaches are the two reserve approaches for such patients. There are certainly some advantages and disadvantages of trans-hepatic and trans-lumbar approaches but is an area of research, further studies, and time to decipher their prospect.
- Bello AK, Okpechi IG, Osman MA, Yeoungjee Cho, Htay Htay, Vivekanand Jha, et al. Epidemiology of haemodialysis outcomes. Nat Rev Nephrol. 2022;18:378–395. Available from: https://doi.org/10.1038/s41581-022-00542-7
- Malviya PB, Andrews R, Ghodke A, Patel B, Reddy A. Percutaneous transhepatic vein permcath: A case report. Indian J Nephrol. 2020;30:430-2. Available from: https://doi.org/10.4103/ijn.ijn_47_20
- Rathod K, Mahajan P, Thakkar D, Jamale T, Deshmukh H. Fluoroscopy and CT Guided Translumbar Tunneled Dialysis Catheter for Hemodialysis Access Failure in a Case of Autosomal Dominant Polycystic Kidney Disease. Indian J Nephrol. 2023;33(1):70-74. Available from: https://doi.org/10.4103/ijn.ijn_429_21
- Murdeshwar HN, Anjum F. Hemodialysis. 2023 Apr 27. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563296/
- Pereira K, Osiason A, Salsamendi J. Vascular access for placement of tunneled dialysis catheters for hemodialysis: A systematic approach and clinical practice algorithm. J Clin Imaging Sci. 2015;5:31. Available from: https://doi.org/10.4103/2156-7514.157858
- Denny DF Jr. Venous access salvage techniques. Tech Vasc Interv Radiol. 2011;14:225-32. Available from: https://doi.org/10.1053/j.tvir.2011.05.006
- Azizkhan RG, Taylor LA, Jaques PF, Mauro MA, Lacey SR. Percutaneous translumbar and transhepatic inferior vena caval catheters for prolonged vascular access in children. J Pediatr Surg. 1992;27:165-9. Available from: https://doi.org/10.1016/0022-3468(92)90305-q
- Wong JK, Sadler DJ, McCarthy M, Saliken JC, So CB, Gray RR. Analysis of early failure of tunneled hemodialysis catheters. AJR Am J Roentgenol. 2002;179:357-63. Available from: https://doi.org/10.2214/ajr.179.2.1790357
- Funaki B. Central venous access: A primer for the diagnostic radiologist. AJR Am J Roentgenol. 2002;179:309-18. Available from: https://doi.org/10.2214/ajr.179.2.1790309
- Po CL, Koolpe HA, Allen S, Alvez LD, Raja RM. Transhepatic perm cath for hemodialysis. Am J Kidney Dis. 1994;24:590-591. Available from: https://doi.org/10.1016/s0272-6386(12)80218-6
- Stavropoulos SW, Pan JJ, Clark TW, Soulen MC, Shlansky-Goldberg RD, Itkin M, et al. Percutaneous transhepatic venous access for hemodialysis. J Vasc Interv Radiol. 2003;14(9 Pt 1):1187-90. Available from: https://doi.org/10.1097/01.rvi.0000085770.63355.f2
- Younes HK, Pettigrew CD, Anaya-Ayala JE, Soltes G, Saad WE, Davies MG, et al. Transhepatic hemodialysis catheters: Functional outcome and comparison between early and late failure. J Vasc Interv Radiol. 2011;22:183-91. Available from: https://doi.org/10.1016/j.jvir.2010.10.011
- Khallaf OAN, Abd El Tawab KA, Korashi HI, Ghada Samir Ibrahim, Rasha Samir Mohamed. Percutaneous transhepatic hemodialysis catheters in chronic hemodialysis patients: technique, functional outcome, and complications from a large population study. Egypt J Radiol Nucl Med. 2019;50:82. Available from: https://doi.org/10.1186/s43055-019-0074-z
- Smith TP, Ryan JM, Reddan DN. Transhepatic catheter access for hemodialysis. Radiology. 2004;232:246-51. Available from: http://dx.doi.org/10.1016/S0749-4041(08)70211-2
- da Motta-Leal-Filho JM, Carnevale FC, Nasser F, de Oliveira Sousa Junior W, Zurstrassen CE, Moreira AM, et al. Percutaneous transhepatic venous access for hemodialysis: an alternative route for patients with end-stage renal failure. J Vasc Bras. 2010;9(3):131.
- El Gharib M, Niazi G, Makkeyah WHY. Transhepatic venous catheters for hemodialysis. Egypt J Radiol Nucl Med. 2014;45(2):431-438. Available from: https://doi.org/10.1016/j.ejrnm.2014.01.008